
If you’ve been stressed, overthinking, or running on fumes, it can start to feel personal, like you’re failing at life. You’re not. Your brain is adapting to what it’s been carrying.
Real mental wellness isn’t hype or luxury. It’s steady inputs that change biology and behavior over time, even when life is still busy and imperfect.
This guide covers supportive habits that tend to improve day-to-day mental health. It isn’t a replacement for therapy, medication, or professional care. Think of it as building a stable “base layer” so your mind has more room to breathe. Small changes compound, consistency beats intensity, and shame helps nothing.
https://www.youtube.com/watch?v=cAYLdBxLoVo
What self-care is (and what it isn’t)
Self-care isn’t a spa day or a perfect morning routine. It’s repeatable actions that reduce your stress load and improve how you function. Sometimes it feels comforting. Often it feels plain.
Comfort can soothe. Care helps you operate better.
A simple definition you can test in real life
Here’s a rule you can use today:
If a habit helps you function better tomorrow, it’s probably self-care. If it only numbs you today, it may be comfort.
You can “test” a habit by watching for signals like:
- A steadier mood (fewer emotional whiplash days)
- Better focus and follow-through
- More patience with people you love
- Fewer crash days after pushing hard
- More willingness to connect, not isolate
Comfort isn’t bad. It just shouldn’t be your only tool.
The science of self-care in plain language
When stress stays high, the body spends more time in “go mode” (sympathetic nervous system). That can raise muscle tension, keep your mind scanning for danger, and make sleep lighter.
Self-care practices work when they help the body shift into “recover mode” (parasympathetic nervous system), and when they support your daily rhythm. Your brain and body like patterns: light in the morning, dim evenings, regular meals, movement, and enough rest.
You’ll hear a lot about brain chemicals online. But neurotransmitters are mostly outputs, not goals. You don’t force serotonin with a hack. You build conditions that support steadier sleep, energy, and connection, and the chemistry tends to follow.
For some people, chronic stress is also linked with inflammation and immune signaling changes. That doesn’t mean “inflammation is the cause of everything.” It means your body systems talk to each other, and lifestyle inputs can matter.
For a broad public health view of stress and coping, see the CDC’s guidance on managing stress.
Myths that keep people stuck (without shaming)
- “If I’m still anxious, self-care isn’t working.” Progress often looks like faster recovery, fewer spirals, and better sleep, not zero stress.
- “Self-care means being calm all the time.” A healthy nervous system still reacts. It just returns to baseline sooner.
- “If it’s free, it can’t help.” Morning light, walking, and bedtime consistency are low-cost and high-impact for many.
- “If it’s popular, it must be evidence-based.” Popularity is marketing, not research.
Safety and scope: when self-care isn’t enough
Self-care can support you, but some situations need prompt professional help. Seek support soon if you notice:
- Thoughts of self-harm or feeling unsafe
- You can’t function at work, school, or home
- Panic feels unmanageable or is escalating
- Substance use is rising fast
- Trauma symptoms are intensifying (nightmares, flashbacks, severe avoidance)
If you’re in the U.S., you can call or text 988 for immediate crisis support.
The five pillars of evidence-based self-care (the big rocks)
Most daily mental health improvement comes back to a small set of basics. These pillars aren’t trendy, but they’re reliable. They support Mental wellness by lowering stress load, improving sleep and mood stability, and making it easier to handle normal life pressures.
If you want a broader, holistic structure that includes spiritual health as well, you can Watch Dr. Deepa’s 6-Pillar Training for Wellness.
For readers who like to see how research reviews self-care tools for anxiety and depression, this open-access paper is a helpful overview: Self-care for anxiety and depression (NCBI).
Pillar 1: Sleep and circadian rhythm (the foundation)
Sleep isn’t a perfection project. It’s the fastest way to change baseline reactivity for many people.
If your sleep is off, everything feels louder: emotions, cravings, worries, and conflict.
Why sleep supports mental health
Sleep supports emotion regulation, threat detection, memory, appetite cues, and impulse control. When sleep is short or fragmented, the brain becomes more reactive, and small stressors can feel huge.
What the research points to (high-level)
Hours matter, but regularity is a strong anchor. A consistent wake time helps set your internal clock. Morning light strengthens that signal, and dimmer evenings help the brain release sleep-related hormones on time. Depth and continuity matter too, not only total time in bed.
Practical sleep habits you can actually repeat
Choose one or two. That’s enough.
- Get 10 minutes of outdoor light early in the day (even on cloudy days).
- Keep a steady wake time most days, including weekends (within 30 to 60 minutes).
- Set a caffeine “last call.” Many people do better stopping 8 to 10 hours before bed, but personalize it.
- Create a boring wind-down (same few steps nightly: shower, pajamas, dim lights, simple reading).
- Cool, dark, quiet basics: lower the room temp, reduce light, reduce noise.
- Stimulus control: if you’re awake in bed for a long time, get up and do something calm, return when sleepy.
- Nap with care: if insomnia is an issue, keep naps short (15 to 30 minutes) and earlier in the day.
- Reduce late-night scrolling: bright light plus emotional content is a rough combo for sleep.
Common obstacles and kind solutions
Parents, shift workers, chronic pain, menopause, and stress spikes can wreck sleep. That’s real. Aim for a “good-enough sleep plan”:
- Protect wake time when you can.
- Add morning light on your first available break.
- If nights are rough, focus on a calmer evening and safe rest, even if sleep isn’t perfect.
Don’t grade yourself. Use sleep as feedback, not a moral score.
Mini checklist: if you change only one thing
- Consistent wake time
- Morning light
- Less late-night scrolling
Pillar 2: Movement (dose matters more than intensity)
Movement is a nervous system tool, not a punishment. It can lower stress tension, support sleep, and build a quiet kind of confidence: “I can do hard things.”
Why movement supports mental health
Regular movement improves stress tolerance and sleep quality for many. It can also support insulin sensitivity and inflammatory balance, which can affect energy and mood in some people.
What to emphasize so it feels doable
You don’t need high intensity. A minimum effective dose exists, and walking counts. Strength work counts. Gentle mobility counts. If you can add daylight or nature, that’s a bonus, not a requirement.
Practical options (low-friction ideas)
- A 10-minute walk after a meal
- “Movement snacks” (2 to 5 minutes): one flight of stairs, 5 squats, a short stretch
- Basic strength 2 days per week (bodyweight is fine)
- Gentle yoga or mobility if your body tolerates it
Barriers and modifications
Depression inertia, fatigue, pain, disability, and chronic illness are real barriers. Try friction reducers:
- Shoes by the door
- A tiny goal (2 minutes still counts)
- Music or a podcast for momentum
- Break it into 2-minute blocks
- Sit-to-stand reps from a sturdy chair
Pillar 3: Food and hydration (stability, not perfection)
Food affects mood partly through energy stability. This isn’t about being “good.” It’s about reducing preventable crashes.
If you have an eating disorder history, strict rules can backfire. In that case, prioritize regular eating and get specialized support.
Why food and hydration can affect mood
Blood sugar swings can mimic anxiety: shakiness, irritability, racing thoughts, and a sense of urgency. Hydration also matters for headaches, fatigue, and focus.
Gut-brain signaling is real, but it isn’t magic. Food can support your baseline, but it won’t erase grief, trauma, or an unsafe life situation.
Evidence-based direction (grounded and simple)
Many people do better with regular meals, enough protein, and more fiber-rich foods. Ultra-processed foods and alcohol can worsen sleep and anxiety for some.
Practical habits that don’t require a new personality
- Add protein to breakfast (eggs, yogurt, tofu, cottage cheese, protein smoothie).
- Create a default lunch you can repeat.
- Pair hydration with cues (after the bathroom, with coffee, before each meal).
- Do an alcohol check-in: notice next-day mood, sleep quality, and baseline anxiety.
- Use “add before subtract” most days (add fruit, add beans, add protein, add water).
For additional ideas framed as everyday self-care, this roundup is a decent starting point: 10 evidence-based tips to improve mental health.
Pillar 4: Connection and relationships (a protective factor)
Humans co-regulate. That means another safe nervous system can help your nervous system settle. It’s not weakness. It’s biology.
Why connection helps mental health
Supportive relationships reduce perceived threat and lower stress load. Loneliness, on the other hand, tends to amplify stress and worsen mood over time.
What counts as connection (it’s more than big social plans)
One safe person counts. A brief voice note counts. A familiar barista counts. So do structured communities like volunteering, clubs, and faith groups.
Quality and safety matter more than quantity.
Practical ways to build connection this week
- Send two low-pressure texts to someone safe.
- Choose a walk-and-talk instead of a sit-down plan.
- Use a simple script on low days: “I’m having a rough day. Can you check in tonight?”
- Practice repair: a small apology, a clear ask, or a kind boundary.
Pillar 5: Skills for the mind (psych tools that hold up over time)
You can’t think your way out of every feeling. But you can change your relationship with your thoughts, and that changes your stress response.
If you have a trauma history, some practices (like eyes-closed meditation) can feel activating. Alternatives are allowed.
Why mind skills matter for mental wellness
Rumination is like a hamster wheel that burns energy without solving the problem. Skills help you notice thoughts without getting dragged by them. They also make behavior change easier, because you stop waiting for motivation to feel perfect.
Tools with strong support (pick what fits)
- CBT-style thought work (labeling, checking, reframing)
- Behavioral activation (action before motivation)
- Mindfulness as attention training (not “empty your mind”)
- Self-compassion as anti-shame and pro-action
- Structured journaling prompts (short, focused)
Simple exercises (step-by-step)
- 60-second “name the feeling” drill:
Name the emotion, rate it 0 to 10, then name one need (rest, food, reassurance, movement, help). - 3-column thought check:
Situation, automatic thought, alternative thought that’s more balanced and still true. - “Next right step” list:
Write one action, one support, one rest item. Do the smallest one first.
Wellness trends vs evidence-based self-care: what often doesn’t improve mental health
Some things feel like relief but quietly raise stress later.
Quick relief that can backfire
Doomscrolling, avoidance disguised as rest, and retail therapy loops can give a short dopamine hit. The cost is often less sleep, more guilt, and less time for the habits that actually help.
Over-scheduling “wellness tasks” can backfire too. When self-care becomes a second job, your nervous system doesn’t read it as care.
Substances and mood (clear facts, no moral tone)
Alcohol fragments sleep and can worsen next-day anxiety for many people. Nicotine can lock you into an anxiety cycle (withdrawal feels like stress, so you smoke again). Cannabis varies by person, but it can worsen sleep quality, motivation, or anxiety for some.
If use is rising, that’s a sign to get support, not a reason for shame.
How to tell if a habit helps (simple metrics)
Use a 1-week experiment. Watch for:
- Better sleep quality
- More stable mood the next day
- Less reactivity
- Better focus
- More willingness to connect
- Fewer crash days
Build a personal self-care plan that fits real life
The goal isn’t a perfect routine. It’s a plan you can do on a hard week.
Start with the highest-return change
Pick one pillar, one habit, one week.
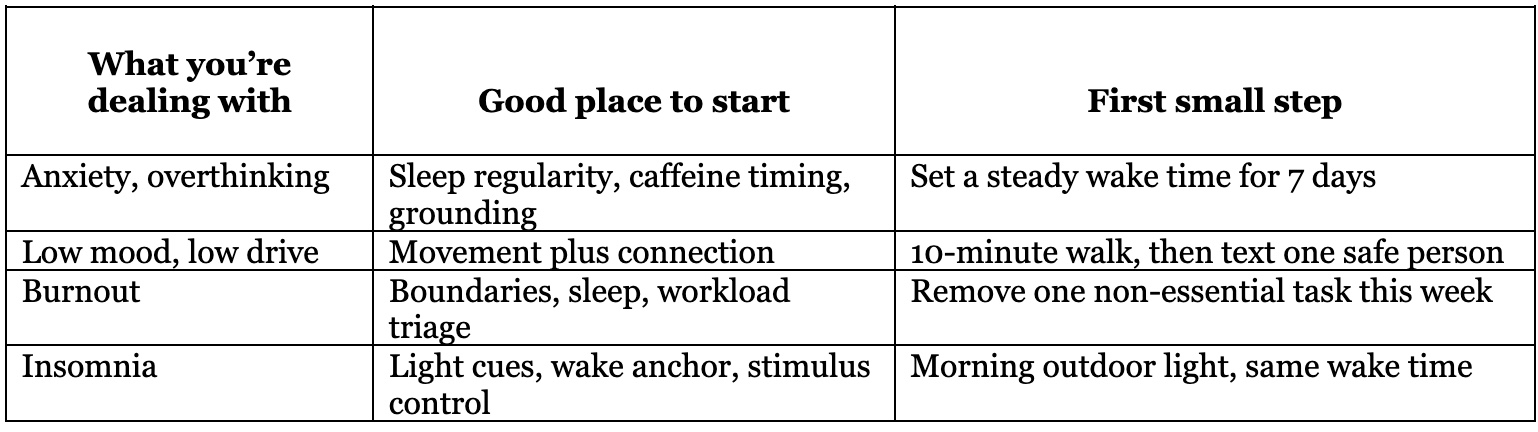
Here’s a simple match-by-symptom guide:
The minimum effective routine (3 levels)
- Level 1 (2 to 5 minutes/day): light, water, one short walk or stretch
- Level 2 (10 to 20 minutes/day): walk plus a simple wind-down
- Level 3 (30 to 60 minutes/day): movement, meal prep basics, longer connection time
Level 1 still counts during hard seasons.
Self-care during flare-ups (an acute stress plan)
When you’re maxed out, go back to basics:
Water, food, sunlight, a 5-minute walk, text one person, basic hygiene.
Do less, then rebuild.
When self-care isn’t enough and what to do next
Step up support when symptoms last weeks, impair your life, or keep worsening.
Options include therapy (CBT, ACT, trauma-informed therapy), group support, and medication as one tool. If you’re talking to a clinician, try:
- “These are my symptoms.”
- “This is how long it’s been happening.”
- “This is how it affects sleep, work, and relationships.”
- “Here’s what I’ve tried.”
- “I’d like help with next steps.”
Special considerations (so this doesn’t feel one-size-fits-all)
Burnout and chronic stress
Burnout is often a load problem, not a character flaw. Rest helps, but so does reducing the ongoing drain. A small boundary script can be enough to start: “I can’t take that on this week.”
Trauma history
Prioritize safety and pacing. Try options that keep you oriented: walking, rhythmic movement, naming five things you see, breathing with eyes open.
Hormonal windows and life stages
PMS, perimenopause, and postpartum seasons can shift sleep and mood. Track patterns gently, protect sleep when possible, and talk with a clinician if symptoms are severe or disruptive.
Neurodivergence and executive function
Use external supports: timers, visual cues, body doubling, and routine anchors. This is about setting up your environment, not trying harder.
FAQs
How long does it take to feel a mental health improvement?
Some people notice sleep and mood shifts within 1 to 2 weeks, especially with a steady wake time and daily light. Deeper change often takes longer because life stressors and habits take time to reset.
What if I can’t stay consistent?
Lower the bar until it’s doable. Consistency grows from small wins, not big plans.
Is self-care the same as therapy?
No. Self-care supports your baseline. Therapy helps you treat patterns, trauma, and ongoing symptoms at the roots.
Does meditation help everyone?
No. If it increases distress, try walking mindfulness, grounding with senses, or a short, eyes-open practice.
What’s the fastest pillar to start with?
Sleep timing and morning light are high returns for many people, especially if anxiety and irritability are high.
Conclusion
If your mind has been loud lately, that doesn’t mean you’re broken. It means your system has been carrying a lot. Mental wellness improves when you give your body steady signals of safety: sleep rhythm, movement, stable meals, real connection, and a few mind skills that reduce rumination.
Pick one small habit for one week. Let it be simple. Then build from there.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.
