
If you feel fine outside but start sniffling the minute you get home, you’re not imagining it. Indoor allergies are common, and they can make your own house feel like the problem.
Most indoor symptoms come from three sources: dust mites, pets, and mold. The goal isn’t a perfect home. It’s lowering your “allergen load,” so your immune system can settle down. When that load drops, many people notice fewer symptoms and better sleep.
Typical signs include a stuffy or runny nose, itchy or watery eyes, coughing, postnasal drip, and sometimes wheezing. Winter can feel worse (and January is a prime time for it) because windows stay shut, air gets recirculated, and we spend more hours indoors.
What Indoor Allergies Look Like in Real Life (and Why Your Body Reacts)
An allergy is basically a false alarm. Your immune system treats something harmless (like dust mite particles or pet proteins) as a threat. Your body releases histamine and other chemicals, which trigger swelling and extra mucus in your nose and sinuses. Eyes can itch and water. Airways can tighten if you also have asthma tendencies.
One reason indoor allergies drag on is exposure. If you’re reacting to something in your bedroom, you’re breathing it in for 7 to 9 hours a night. That’s like poking a bruise over and over and wondering why it stays sore.
It also helps to separate allergies from irritants. Strong smells, smoke, and cleaning fumes can cause burning eyes, coughing, or a runny nose, but that’s irritation, not an immune reaction. The fix there is often ventilation and avoiding triggers, not allergy meds.
For a practical medical overview of common indoor triggers, see the American Academy of Allergy, Asthma, and Immunology guide on indoor allergens.
Allergy or Cold? A Quick Way to Tell The Difference
Use this as a quick reality check. It’s not perfect, but it’s useful.
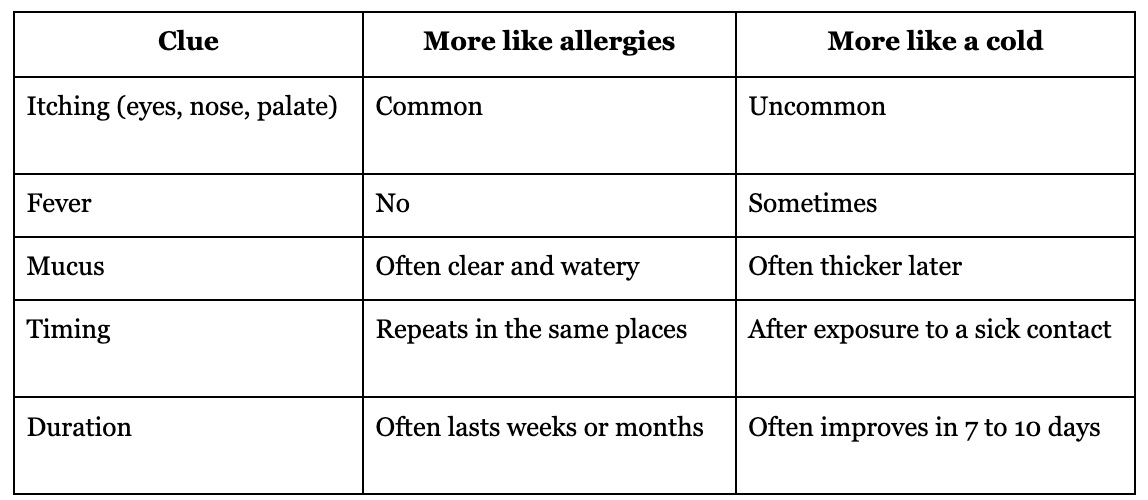
Both can overlap. If symptoms keep returning, last more than 2 weeks, or keep you up at night, it’s worth getting checked.
Why Indoor Symptoms Can Feel Worse at Night and in Winter
Nighttime symptoms often point to the bedroom: pillows, mattresses, carpet, and dusty fabric surfaces. Lying flat can also make congestion and postnasal drip feel stronger.
In winter, homes are sealed up. That can trap allergens inside and reduce fresh-air dilution. Humidity swings matter too. Dust mites and many molds do better when indoor humidity stays high, so the same home can feel fine one week and rough the next.
Meet the “Big Three” Indoor Triggers: Dust Mites, Pets, and Mold (and Where They Hide)
You don’t need to overhaul your whole house this weekend. Start where you spend the most time and where symptoms hit hardest. For many people, that’s the bedroom.
The “big three” triggers act differently:
- Dust mites build up in soft, warm places.
- Pet allergens spread through the whole home and cling to fabrics.
- Mold is a moisture issue first and an allergy issue second.
If you want a deeper medical explanation of why dust mites cause symptoms and where they commonly live, Mayo Clinic’s overview on dust mite allergy symptoms and causes is a clear resource.
Dust Mites: The Invisible Bedroom Roommate
People aren’t usually allergic to the mites themselves. They react to proteins in mite waste and tiny body fragments. Mites love mattresses, pillows, bedding, upholstered furniture, and carpet.
Higher humidity, lots of fabric surfaces, and plush toys increase the odds. The basics that tend to help most are consistent: allergen-proof covers, weekly hot washing, and HEPA-grade vacuuming.
Pet dander: It’s Not The Fur; It’s The Flakes and Saliva Proteins
Pet allergens come from skin flakes, saliva, and urine proteins. Fur carries those proteins around, but fur isn’t the real trigger. Dander settles into carpets, couches, and blankets, and it can stay in dust even when your pet isn’t in the room.
Also, “hypoallergenic” pets aren’t truly non-allergenic. Some people tolerate certain breeds better, but no breed is a guarantee.
If you love your pet, you’re not alone. The aim is boundaries and cleaning habits that lower exposure, not shame.
Mold: A Moisture Problem First, An Allergy Problem Second
Mold releases spores into the air. When there’s moisture, mold can grow behind walls, under sinks, around windows, and in bathrooms, basements, and HVAC drip areas.
Small surface spots can sometimes be cleaned safely, but large areas, repeated regrowth, or ongoing water damage often need professional remediation. If you’re seeing stains spread, smelling a musty odor that won’t quit, or dealing with leaks, address the moisture source first.
What Actually Helps: A Simple Plan You Can Do This Week
Big improvements often come from boring consistency. Small steps done weekly beat a once-a-year deep clean.
If you want personal guidance and medical support beyond DIY steps, consider Allergy & Immunology Services by Dr. Deepa Grandon. Dr. Deepa Grandon is a triple board-certified physician with 23+ years of experience and offers comprehensive telehealth evaluations across all 50 states.
Start in the Bedroom for the Biggest Payoff
- Zip up the bed: Use zippered allergen-proof covers for the mattress and pillows.
- Wash weekly: Wash sheets and pillowcases weekly in hot water (about 130°F if the fabric allows), then dry fully.
- Reduce fabric clutter: Fewer throw pillows, fewer heavy blankets, and fewer dust-catchers near the bed.
- Refresh old pillows: Consider replacing pillows every 2 to 3 years.
- Handle stuffed animals: Hot wash if possible, or freeze for 24 hours, then wash to remove allergens.
If carpet is a big trigger and changing flooring isn’t realistic, focus on the bed first. It’s the highest exposure zone.
Control Humidity and Airflow (the 30 to 50% Rule)
Aim for 30 to 50% indoor humidity. Too high feeds dust mites and mold. Too low can dry out nasal passages and make you feel stuffed up anyway.
- Measure it: A small hygrometer is cheap and takes the guesswork out.
- Lower humidity: Use a dehumidifier, run bathroom fans during showers, fix leaks fast, and don’t vent dryers indoors.
- HVAC basics: Change filters every 60 to 90 days (more often with pets). Use higher filtration if your system allows it, and keep vents unblocked.
- Air purifiers: A HEPA air purifier can help, especially in bedrooms, but it works best paired with source control (bed covers, washing, humidity).
For practical home steps and a room-by-room mindset, AAFA’s guide on controlling indoor allergens is a solid reference.
Cleaning That Works (and What Does Not)
Vacuum 1 to 2 times per week with a HEPA vacuum if you can. Damp-dust hard surfaces instead of dry dusting, which tosses particles back into the air. Mop hard floors, and wash pet bedding often.
Common mistakes that backfire:
- Dry dusting or feather dusters
- Scented candles and sprays, which can irritate sensitive airways
- “Miracle” gadgets that promise to remove all allergens without cleaning
Busy schedule? A focused 10-minute routine still matters. Do the bedroom floor, wipe nightstands, and swap pillowcases. Consistency is what changes symptoms.
Relief Options: Over-the-Counter Meds, Prescriptions, and When To Get Tested
Home steps lower the trigger load, but many people still need medication, at least during flares. Often, the best plan is both: reduce exposure, then treat symptoms.
For a balanced, evidence-based overview of dust mite allergy care, including medical treatment options, see this NCBI overview of dust mite allergies.
OTC Choices That Help Most People Breathe and Sleep Better
- Non-drowsy oral antihistamines: Often help with sneezing and itching.
- Steroid nasal sprays: One of the strongest first-line options for congestion, but they work best when used daily for several days to weeks.
- Saline rinses or sprays: Helpful for thick mucus and postnasal drip.
- Allergy eye drops: Can calm itchy, watery eyes quickly.
Use decongestants with care. Some raise blood pressure or trigger jitters. And topical decongestant sprays can cause rebound congestion if used too long. Follow labels, and ask a clinician if you’re pregnant, treating a child, or managing conditions like high blood pressure, glaucoma, or prostate issues.
When It’s Time to See a Clinician (and What You Can Ask for)
Get medical support if:
- Symptoms last more than 2 weeks
- Sleep keeps getting disrupted
- You wheeze, feel short of breath, or cough at night
- You’re getting frequent sinus infections
- OTC meds and home steps aren’t helping
You can ask about allergy testing to confirm triggers, prescription nasal sprays or inhalers when needed, and immunotherapy (shots or under-the-tongue options, depending on the allergen and your clinician).
A simple visit prep list: your symptom pattern (where and when), home exposures (pets, basement, carpet), what meds you tried, and your typical humidity readings if you have them.
Key Takeaways
Indoor allergies are a common immune response, not a personal failure. Start with the basics: focus on the bedroom, keep humidity in the 30 to 50% range, clean with HEPA tools, then add targeted meds if needed. Pick one change today, track symptoms for 2 to 3 weeks, and adjust from there. If breathing symptoms show up, sleep stays disrupted, or problems keep returning, it’s time to get medical support.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.

