
That scratchy throat, the runny nose, the nonstop sneezing. When you feel “off,” it’s hard to know if you’re dealing with allergies vs. cold because the first few symptoms can look almost the same.
The good news is that your body usually leaves clues. You don’t need a medical degree to spot them, you just need the right questions.
This quick guide gives you a simple 60-second check to help you choose your next step (self-care, allergy support, or getting checked). It’s not a substitute for medical care, especially if you have warning signs or chronic lung issues.
The 60-second self-check you can do right now
Grab a tissue and do this fast scan. Answer each question with your best “yes” or “no.”
- Do your eyes or nose feel truly itchy? (Not just irritated.)
- Do you have a fever or chills?
- Do you have body aches or that “hit by a truck” feeling?
- Did symptoms start suddenly right after a trigger (outdoors, cleaning, pets, dusty room)?
- Has it lasted more than a week without improving?
- Are you around people who’ve been sick lately (household, coworker, classroom)?
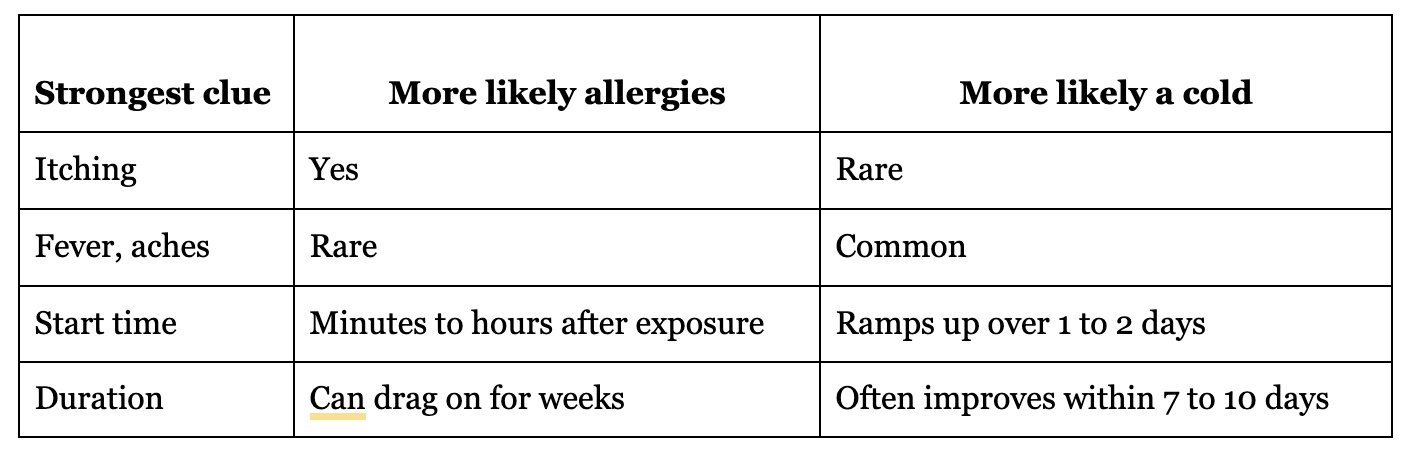
A quick way to interpret your answers:
If you want a clinician-reviewed overview of classic differences, Mayo Clinic's breakdown of cold vs. allergy symptoms is a solid reference.
Itchy eyes or itchy nose usually points to allergies
Itch is one of the most useful “tells.” Allergies trigger your immune system to release histamine. Histamine is what makes your eyes water, your nose itch, and your skin feel prickly.
Common allergy patterns include:
- Itchy, watery eyes that make you want to rub them all day
- Itchy nose or roof of mouth, sometimes an itchy throat
- Sneezing fits that come in bursts, especially when you first walk outside
- A clear, watery runny nose, plus post-nasal drip (mucus sliding down the back of your throat)
Colds can cause irritation from swelling and drainage, but true itchiness is less common. If you keep thinking, “My nose feels like it has pepper in it,” allergies move higher on the list.
One more clue: allergies often come with “repeatable misery.” If you feel fine indoors, then flare up every time you’re outside, that pattern matters.
Fever, body aches, and a sore throat usually point to a cold
Colds are caused by viruses. Your immune system responds with inflammation, and that response can make your whole body feel worn out.
Signs that usually lean “cold” include:
- Fever (more common in kids than adults, and often low-grade)
- Body aches, headache, or a heavy fatigue that’s out of proportion to your nose symptoms
- Sore throat early on, especially with swollen glands
- A cough that becomes productive (phlegm) as the days go on
Not every cold comes with fever, but when fever and aches show up together, it’s a strong viral signal. If you’re weighing allergies vs. cold, aches tip the scale toward cold.
Clues that matter most: timing, mucus, and how long it lasts
When you’re stuck in the “I can’t tell” zone, patterns over the next 6 to 48 hours often make it clearer.
Think in scenes:
- You mow the lawn, then within an hour you’re sneezing and your eyes won’t stop watering. That’s a classic allergy setup.
- Your coworker has been coughing all week, then two days later you get a sore throat, fatigue, and a stuffy nose. That’s a common cold story.
- You travel, sleep poorly, touch a lot of surfaces, and then start feeling run down. Viruses love those moments.
Duration matters too. A cold often improves in a week, though a cough can linger. Allergies can hang on for as long as the trigger is around.
Pollen seasons can also be longer in some regions than people expect, especially in milder winters. If symptoms strike “out of nowhere” in January, it may still be allergies in your area, or it may be an indoor trigger like dust or mold. The pattern is still the key.
For a simple public health explanation of overlapping symptoms, NIH has a helpful overview on cold, flu, or allergy differences.
How fast it started, and what you were around, can be the giveaway
Allergies often start quickly after exposure. Sometimes it’s minutes, sometimes a few hours.
Typical triggers include:
- Outdoor: pollen, grass, weeds, yard work, windy days
- Indoor: dust, pet dander, mold, strong scents, smoke
Colds usually have a quieter beginning. You might feel “a little off” at first, then symptoms build over 24 to 48 hours. That delay fits how viruses incubate.
A useful question is, “Did my symptoms show up like a light switch or like a dimmer?” Light switch points to allergies. Dimmer points to a cold.
If symptoms pop up mostly at home, pay attention to the environment. A dusty fan, old pillow, damp bathroom, or new pet can keep the cycle going.
What your mucus is telling you (and what it is not)
Mucus gets blamed for everything, but it’s easy to misread.
Allergies often cause:
- Clear, watery drainage
- Lots of sneezing
- Post-nasal drip that leads to a dry cough, especially at night
Colds can start with clear drainage too. Over a few days, mucus may get thicker and look cloudy, yellow, or green.
Here’s the part many people don’t hear enough: green mucus doesn’t automatically mean you need antibiotics. Color can change during a viral infection as immune cells build up in the mucus. What matters more is the overall story: Are you improving, staying the same, or getting worse?
If you want a clinician-friendly explanation of how symptoms tend to differ, Mayo Clinic Health System’s guide on allergy vs. common cold signs is a practical read.
Red flags that deserve medical attention include worsening facial pain with fever, shortness of breath, chest pain, or symptoms that sharply worsen after you seem to improve.
What to do next, and when it’s time to get medical help
Once you’ve made your best guess, aim for low-risk steps that match the most likely cause. You can also hedge a bit. For example, using saline rinses and prioritizing rest can help either way.
If you’d like physician-led support without waiting rooms, Transformational Life Consulting Medical Division offers telehealth medical consultations and allergy-focused care led by Dr. Deepa Grandon (triple board-certified physician with 23+ years of experience).
Here’s when to skip home troubleshooting and get checked sooner:
- Trouble breathing, wheezing, or asthma flare that isn’t settling
- Chest pain, fainting, confusion, blue lips, or severe weakness
- Dehydration (very little urine, dizziness, unable to keep fluids down)
- Fever that’s high, persistent, or paired with stiff neck or severe headache
- Symptoms lasting more than 10 to 14 days without clear improvement
- New symptoms after initial improvement (sometimes called “double sickening”)
- Infants, older adults, pregnancy, or significant immune problems, because the risk math changes
If it looks like allergies, try these first steps for quick relief
Start with the basics that reduce exposure and calm inflammation.
Tidy up the trigger path: If you’ve been outdoors, shower and change clothes. Rinse pollen from hair and eyelashes. Keep bedroom air clean, and avoid letting pets sleep on the pillow if pet dander is a trigger.
Saline rinse: A simple saline spray or rinse can wash out irritants and thin mucus. Use sterile or distilled water if you’re doing a rinse bottle or neti pot.
Non-drowsy antihistamine: Many people do well with a once-daily, non-sedating option. If you’re pregnant, have glaucoma, have urinary retention issues, or take other meds, check with a clinician first.
Steroid nasal spray: For frequent symptoms, a daily nasal steroid spray can reduce swelling and drip. It works best when used consistently for several days, not just once.
Control the air: Keep windows closed on high pollen days, run a HEPA filter if you have one, and avoid outdoor chores when counts are high.
If you have asthma, allergies can trigger coughing, wheezing, and chest tightness. Use your action plan and rescue inhaler as directed. If you don’t have a plan, that’s a good reason to schedule a visit.
If it looks like a cold, focus on support, rest, and protecting others
For most healthy people, a cold is miserable but self-limited. The main job is to support your body and limit spread.
Rest and fluids: Sleep is not laziness here; it’s repair time. Sip water, broth, or warm tea.
Soothe the throat: Salt-water gargles can help. Warm fluids often feel better than cold ones.
Honey for cough: Honey can reduce cough frequency in adults and older children, but don’t give honey to babies under 12 months.
Fever and pain relief: Acetaminophen or ibuprofen can help if you can take them safely. Follow label directions and consider your medical history (ulcers, kidney disease, liver disease, blood thinners).
Protect other people: Wash hands well, avoid sharing drinks, and stay home when you’re actively sick if possible. Viruses spread fast before you even feel your worst.
Call a clinician if symptoms last beyond 10 to 14 days, you have ear pain, you’re short of breath, or you’re getting worse after a brief improvement. Those patterns can point to complications like an ear infection, sinus infection, or pneumonia, especially in kids and older adults.
Key Takeaways
When you’re deciding between allergies vs. cold, focus on the quickest differentiators: itchiness and long-lasting, repeatable symptoms often suggest allergies, while fever, body aches, and a shorter course usually suggest a cold.
Give it 24 hours of observation if you’re not sure. Track your symptoms, note any triggers, and treat the most likely cause with low-risk steps.
If red flags show up or you’re not improving, getting medical guidance is the smart move, not an overreaction.
Ready to take control of your allergies? Sign up for our telehealth waitlist to meet with Dr. Deepa over video call by clicking here.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.

